Background:Sickle cell disease (SCD) is a chronic multisystem disorder associated with vaso-occlusive pain and organ damage, leading to substantial morbidity, impaired health-related quality of life, increased health care costs, and a high risk of premature death (Platt el al. N Engl J Med. 1994). SCD complications and pain episodes accounted for 23% of statewide admissions, mainly by a small group of high utilizers. (Woods et al. Public Health Rep, 1997). Adults with SCD have a high rate of depression, 35% compared to 6.7% in the general adult population (Adam, Flahiff, Kamble, et al. 2017). Chronic persistent pain occurs in more than a third of adults with SCD. Opioid analgesics, the mainstay for the management of acute and chronic pain, often results in opiate use disorder (Ehrentraut et al. J Pediatr Psychol. 2014). Current clinical approaches to address depressive symptoms in SCD have not been effective due to the gaps in care and barriers to access healthcare resources. Client-centered (or person-centered) therapy, is a non-directive approach to counseling that incorporates the concepts of unconditional positive regard, empathetic understanding, genuine affect, and culturally responsive care to improve psychosocial outcomes (Meyer & Zane, 2018). We sought to address these perceived gaps in care using client-centered therapy to improve patient related health outcomes in a cohort of adult patient who were high utilizers.
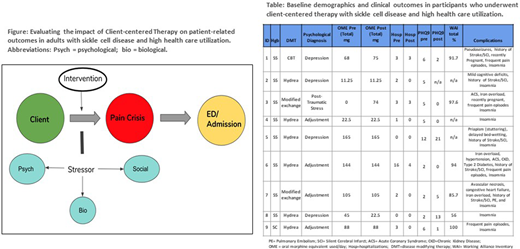
Methods:The study sample comprised 9 patients with SCD (HbSS and SC), ages 23-42, who followed with the adult SCD Clinic at Vanderbilt University Medical Center in Nashville, TN. This cohort of patients was selected as they accounted for the highest health care utilization in our adult program. Demographics and baseline clinic data were obtained on each participant, including pre- and post-measures for hospitalizations, oral morphine equivalent (OME), PHQ-9 to measure depressive symptoms, and the Working Alliance Inventory (WAI), to measure the effectiveness of the client-centered approach to therapy (based on consensus of goals, confidence in and commitment to helping relationship, and mutual trust). Our approach to evaluations is depicted in Figure. Exclusion criteria included current diagnosis of psychosis or a comorbid disorder with psychosis as defined by the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition); active suicidal/homicidal ideation, and unwillingness to participate in counseling. Patients were expected to attend 7 individual sessions for 60 minutes each with a trained mental health clinician. Clinical and laboratory data was obtained through electronic medical record under an IRB approved protocol.
Results:In our sample, 5/9 (56%) of our patients were male and they were all African Americans. Eight out of 9 participants had HbSS and 1 had HbSC. The median age of all participants was 30 years. The participants completed a combined total of 64 sessions over an average of 6.7 months. All participants completed an average of 7 sessions each. The average number of hospitalizations pre-intervention per participant was 3 and decreased to 1 post-intervention. The pre and post OME totals for 6/9 participants remained stable. One participant (#8) had a 50% decrease in OME, and two participants (#2, #3) had an increase in total OME post-intervention associated with pregnancy-related complications. Pre-intervention, 69% of participants identified mild to moderate severity in depressive symptoms. The total PHQ-9 scores decreased post-intervention by 3 points, or by 4.4%. The WAI average post-intervention depicts an average of 87.5% of participants identified a strong working alliance with their therapist (Table).
Conclusion:Our pilot study shows that client-centered therapy is a safe and effective approach to address age-dependent chronic health challenges of adults with SCD. Client-centered therapy decreased hospitalization rates and PHQ-9 scores for our high utilizers. Though there was not a statistically significant decrease in participants' OME, 67% of the sample remained stable, without an OME increase during the intervention period. Future research and longer-term studies are needed on utilizing this approach to address coping mechanisms, baseline stress levels, and overall quality of life in a larger cohort of adults with SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal